|
Special Needs Plans
There are many types of plans depending upon your level of qualification. What is a D SNP? Dual Eligible Special Needs Plans - or D SNP's for short - are a special type of Medicare Advantage plan that provides health benefits for people who are “dual eligible,” meaning they qualify for both Medicare and Medicaid. States determine which D SNP's can be offered and the benefits provided. More Info |
|
Generally speaking, D SNP’s may include:
Vertical Divider
|
A DSNP plan will include coverage for hospital services (Medicare Part A), medical health care needs (Medicare Part B), and prescription drugs (Medicare Part D) through a single plan. With a DSNP there may also be social services
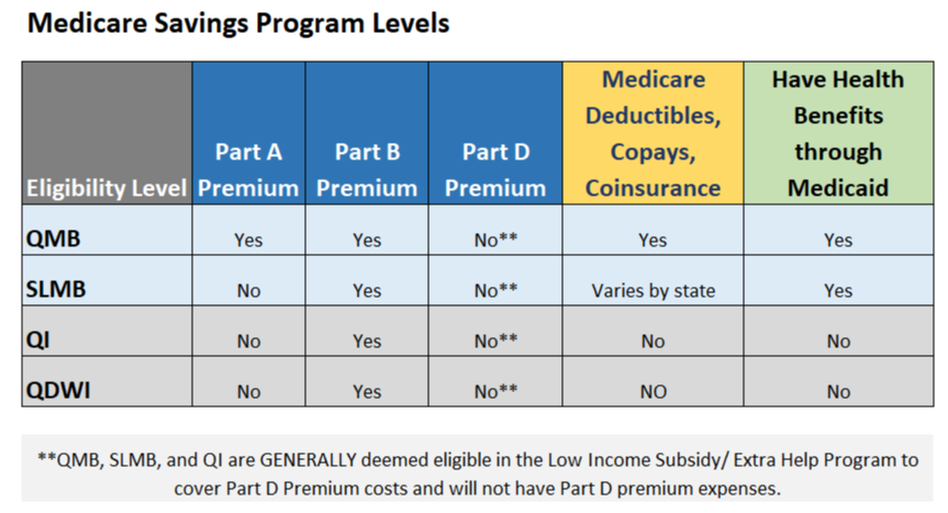
There are five DSNP types with varying degrees of Medicaid coverage:
|
|
Contact DSHS (Dept. Social and Health Health Services)
Washington -
|
Thank You for your information... Next Step, Book Your Appointment...